Patient arrives at ED
A 58-year-old male with a history of hypertension, chronic kidney disease, coronary artery disease, past stents and congestive heart failure presents to the Emergency Department. Over the past four days, he has experienced shortness of breath and a worsening cough that is exacerbated with exertion. He denies any chest or abdominal pain as well as fever and chills.
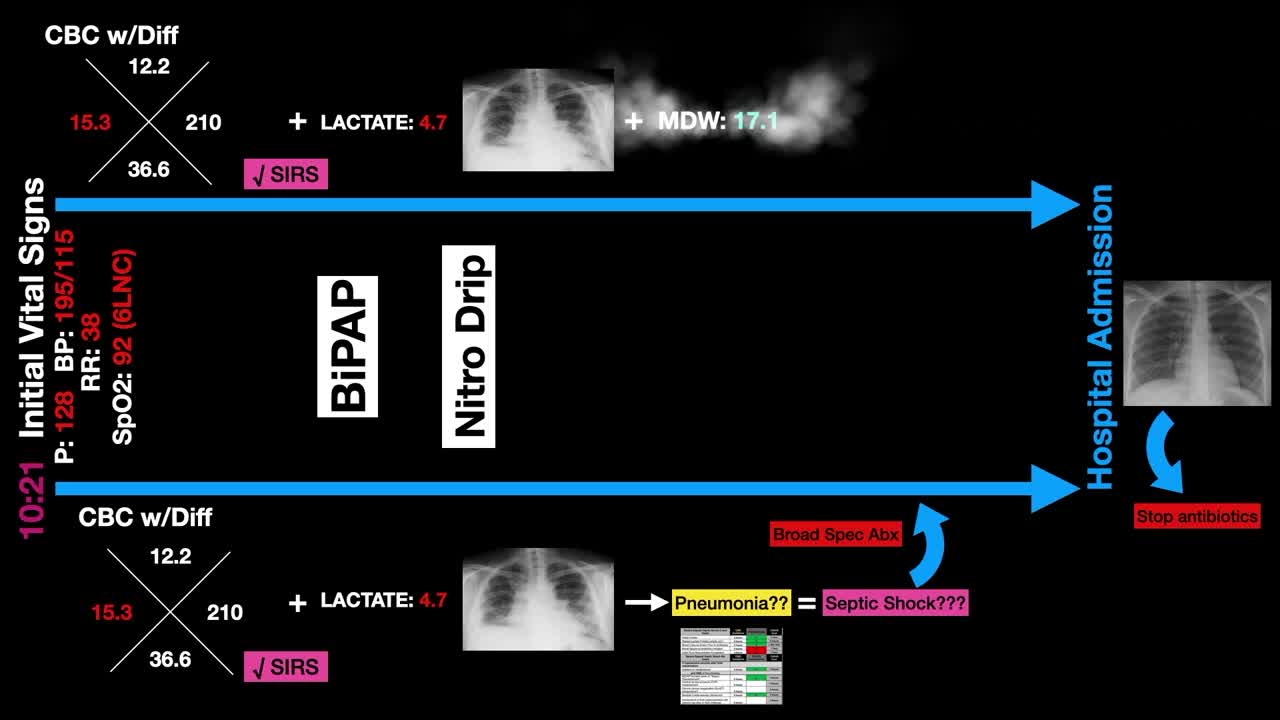
10:21 p.m.
Initial Assessment
Respiratory distress with tachypnea and tachycardia.
T: 37.6 | P: 128 | BP: 195/115 | RR: 38 | SpO2: 92 (6LNC)
All vitals assessed were considered abnormal except for temperature.
10:31 p.m.
Patient’s EKG results show sinus tachycardia without ST changes.
10:45 p.m.
Elevated point of care tests returned
Troponin: 0.06 | BNP: 990
Lactate: 4.7
11:15 p.m.
CBC with Differential resulted
WBC 15.3 | MDW 17.1
11:37 p.m.
BMP resulted:
Elevated creatinine of 2.93, which was up from 2.2 three months prior
BUN of 42.
11:46 p.m.
Chest X-ray findings showed ill-defined opacities in both lungs suggesting pulmonary edema or multifocal pneumonia.
Decision to defer antibiotics
The combination of the patient’s elevated WBC, tachycardia and increased respiratory rate meant that SIRS criteria were met. Moreover, SIRS + Lactate of 4.7 and positive chest x-ray were suggestive of multifocal pneumonia. Despite not having confidence that an infection truly existed, there was pressure to start broad-spectrum antibiotics to ensure SEP-1 fallout did not occur.
However, in this case, the MDW was 17.1 – below the threshold of 20 –decreasing the probability of a sepsis diagnosis. As a result, antibiotics were not started as infection, sepsis and bacteremia were not suspected. Abnormal vital signs, elevated WBC and lactate were attributed to acute decompensated heart failure.
 English
English