CBC Validation
Each time pathologists validate results, they are validating the entire process—from the pre-analytical phase through laboratory testing. Of course, activities in the pre-analytical phase are beyond the control of the laboratory itself, which is why laboratories implement methods to detect spurious results.
Among the tests available in the hematology laboratory, the Complete Blood Count with Differential (CBC-Diff) is the most run test.1,2 Unusual results on a CBC-Diff may trigger other tests including peripheral blood smear review.
Life on the (feathered) edge
The peripheral blood smear is a powerful diagnostic tool that can corroborate and/or enhance the CBC by providing further insights into hematological disorders.3 A classic peripheral blood smear slide can be broken down into three parts—the base, the monolayer, and the feathered edge. The manual differential is generally performed at the monolayer where the morphology is most accurate. But the blood smear’s feathered edge, the thin region of the smear where the cells are spread out amongst large empty spaces, provides an opportunity to view platelet clumping, microfilariae, certain red blood cell (RBC) anomalies, large neoplastic cells, and other large, heavy cells that move to the slide’s end.
What Triggers a Peripheral Blood Smear?
In cases where invalid or abnormal results are identified on the CBC-Diff, further evaluation with the expertise of a hematopathologist is required. Below are some CBC-Diff triggers and situations where evaluation of feathered-edge components might be useful.
White blood cells
Triggers for further evaluation:4
- High (>20 x 103/μL) or low (<4 x 103/μL)
Each WBC subpopulation has its own flag for further evaluation, but overall, numbers that are too high or low trigger PBS review. Abnormally large cells that may be of diagnostic importance have a tendency to move to the feathered edge of the smear.5,6 Infection with Epstein-Barr virus (infectious mononucleosis) can lead to large irregular lymphocytes (conversely, infection with Bordetella pertussis (whooping cough) can lead to smaller lymphocytes).5 WBCs from patients with malignant conditions like Chronic Lymphoid Leukemia (CLL) and Acute Myeloid Leukemia (AML) may concentrate at the feathered edge, and these cells may be distributed less randomly and subsequently missed in a manual review of the slide that does not review the feathered edge.7
Red Blood Cells
Triggers for further evaluation:4
- Hemoglobin levels <7 gr/dL or >18 gr/dL
- Reticulocytes >0.100/µL
- MCV <75 fL or >105 fL
Certain quantitative CBC results trigger the need for review. Similarly, qualitative disorders, such as dimorphic RBCs and sickled cells, require further verification. While normal RBC morphology should not be studied at the blood smear’s feathered edge because abnormal cell morphology can be difficult to see here,8 the feathered edge is the perfect place to view RBC abnormalities such as Howell-Jolly and Pappenheimer bodies, the presence of rouleaux (stacks), and internal cell parasites.9
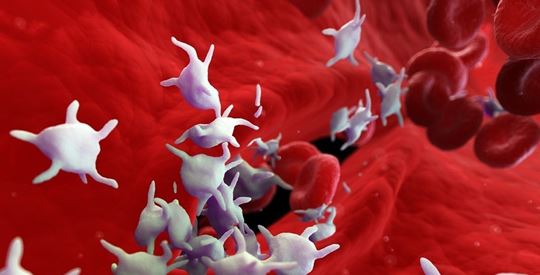
Platelets
Triggers for further evaluation:4
- PLT <100 x 103/µL or PLT >800 X 103/µL
As with WBCs and RBCs, platelet numbers that are too low or too high can trigger the need for PBS review. Low platelet numbers can be seen in conditions such as immune thrombocytopenic purpura,10 where platelet turnover is increased, and in Bernard Soulier Syndrome,11 a problem with platelet adhesion. Both conditions result in the formation of large/giant platelets.
Falsely low platelet counts may be the result of platelet clumping, which can lead to a flag for underestimation of platelet number on an automated platelet count. Platelet clumping can occur due to faulty anticoagulant or because of an old blood sample. When platelet clumps are seen in the feathered edge, a new blood draw may be necessary.12

High platelet counts, thrombocytosis, may occur as a result of a bone marrow disorder (essential thrombocythemia) or in response to a trigger (e.g., hypoxia, infection, injury). Falsely high automated platelet counts can arise from red or white blood cell fragmentation.12
Digital Cell Morphology—Leading through innovation
In today’s hematology laboratory, both workload and patient complexity has increased, but the level of qualified staffing has not. Scopio’s digital cell morphology platform advances in digital cell imaging and facilitates remote review and allows for simplified collaboration. Hematopathologist now have a view of individual abnormal cells in context, which gives a more thorough vision of what’s happening in the patient’s blood.
This innovative technology provides a way to maintain the standard of care with reduced result variability. With full-field digital sample review, clinicians can see the full patient picture from anywhere using the secure hospital network, enabling decentralized medicine to improve collaboration. For example, with Scopio, clumps were detected in the feathered edge in 100% of confirmed pseudothrombocytopenia cases.13
AI-based cellular subclassification has full traceability to assist with rare and unusual disease-related cell types.14 Scopio’s reliable AI decision support system reduces turnaround time for PBS reviews by 60%, representing significant optimization of lab workflows and operational efficiencies.15 Moreover, AI and standardized classification provides unbiased categorization of 16 subclasses of WBCs, providing superior classification over microscopy alone.
Zoom out at the feathered edge to assess the overall quality of the smear and to see abnormally large cells. Zoom halfway to get an overall picture of the cells, identify the presence of RBC rouleaux, and observe platelet clumps. Zoom in fully to see the nuances of the WBCs, the presence of giant platelets, and inclusions in RBCs.
With its reduced review time,13 collaboration power, and superior digital imaging of cells, Scopio’s Full-field Digital Imaging platform is changing peripheral blood smear review.
What’s hidden at the edge? Answers.
Learn more about Scopio’s Full-field Peripheral Blood Smear technology

 English
English