The ED: A Point of Entry for Critical Patients
The clinical priority in the emergency department (ED) is to triage patients quickly, so the most critical receive timely care. As key entry points for many patients entering the healthcare system, EDs can easily become overwhelmed with high caseloads and diminished resources. A pandemic flu season or infectious disease outbreak stretches resources further. Patient flow is crucial to patient care, and clinicians vitally need tools to help them quickly diagnose and decide to treat, release or admit patients.
Because ischemic heart disease is the leading cause of death in men and women globally,1 it is an area of intense focus in the ED. Each year, in the U.S., 8 million patients enter the ED with chest pain.2 Yet almost 95% are not diagnosed with a heart attack or serious condition.3
Rapid detection of acute myocardial infarction (AMI) means moving the patient to the next step in the care pathway for further treatment. Ruling out a cardiac event could allow a patient to be released sooner, making room for others seeking care. A high-sensitive troponin I test gives clinicians fast, accurate information to support early rule in or rule out of AMI in the ED.
Cardiac Troponin: An Important Functional Protein
Troponins are regulatory proteins found in skeletal and cardiac muscle that play a role in muscle contraction. Three types exist, and their differentiation is important when considering a diagnosis of AMI.
- Troponin C is present in both cardiac and skeletal tissue
- Troponin T is also found in both cardiac and skeletal tissue based on subtypes
- Troponin I is cardiac specific
When damage or death of cardiac tissue occurs for any reason, cardiac troponin (cTn) is released into the circulation by cardiac muscle cells. Blood cTn testing, therefore, can serve as a significant piece of the diagnostic puzzle, indicating tissue damage and potentially offering insight into underlying causes. While troponin as a biomarker has been recognized since the late 1980s, in 2000, it emerged as the gold standard for assessing myocardial tissue damage.4
What makes cTn so desirable as a diagnostic biomarker is its characteristics in the setting of cardiac injury. During an MI, for example, a patient’s cTn levels rise sharply and remain elevated over time with a relatively slow decline. Clinicians can, therefore, take serial measurements at close intervals to determine the rise and/or fall of levels for days.
Elevated troponin levels are associated with adverse outcomes,5 and rise/fall patterns indicate acute coronary syndrome (ACS). This is preferred over other cardiac biomarkers that do not show a marked increase and decrease in levels, or other cardiac muscle injuries that may show a steady elevation pattern. These other cardiac injuries include congestive heart failure, myocarditis, atrial fibrillation and catheter ablation. (Figure 1)
Rise in Troponin and Time After Onset of MI
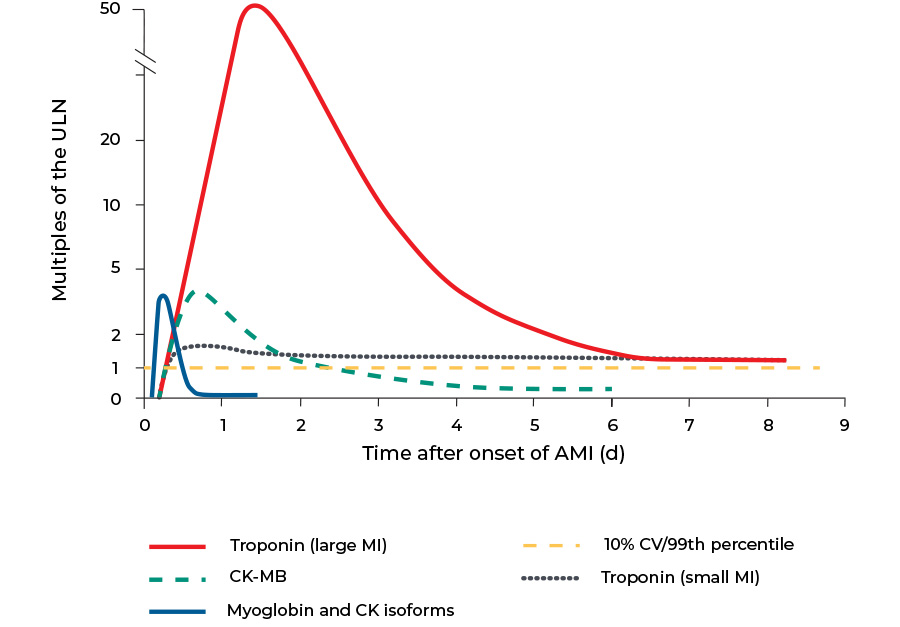
Figure 1. Troponin rises quickly after onset of MI and tapers off over time.
High-sensitivity Troponin Test: Next-level Precision
Next-generation, high-sensitivity cardiac troponin assays emerged globally in 2010; they were introduced to the U.S. market in 2017.6 The following year, the “Fourth Universal Definition of Myocardial Infarction” offered updated guidelines, recommending the use of high-sensitivity cardiac troponin assays that meet International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) precision criteria.5 These tests feature troponin I (hs-cTnI) or troponin T (hs-cTnT). While these tests appear to perform similarly, there is evidence that elevated troponin T levels may be closely related to non-CVD death.7
cTn vs. high-sensitive troponin assays
While high-sensitivity cardiac troponin assays measure the same analyte as their predecessors, they are more precise in analytical sensitivity. A high-sensitive troponin test can measure lower levels of troponin in blood, obtaining limits of detection (LoD) in ranges that were previously undetectable. This allows for the measurement of troponin levels in normal healthy individuals. The high precision offers several advantages:
- Rapid diagnosis or exclusion of AMI within one hour—compared to 12 hours with previous troponin assays6
- Confident results reporting due to a low coefficient of variation (CV—<10% at 99th percentile of the reference population; measurements are reproducible and indicate that rising and falling troponin patterns are due to a patient’s biology, not test imprecision)8
- More accurate calculation of the 99th percentile upper reference limit (URL) with a 95% confidence interval9
- An LoD that is in the single-digit ng/L range and markedly lower than the URL—determined by measuring troponin levels in a healthy reference population9
- Sex-specific reference ranges to address troponin level differences in men and women
- Flexibility to use serum or plasma, depending upon the test
High-sensitivity troponin test reference range
Values for high-sensitivity cardiac troponin assays are reported in whole numbers. Whereas contemporary assays are commonly reported as ng/ml, high-sensitivity assays are reported as pg/ml or ng/L. While this is a marked change for clinicians interpreting results, it is significant, as smaller differences in troponin levels become more apparent.
A high-sensitivity troponin range for men and women
Overall, men and women exhibit different troponin levels, largely due to differences in heart size. Determination of sex-specific reference ranges are possible with high-sensitivity cardiac troponin assays. This may help refine identification of AMI in women, who often present with atypical symptoms.
Implementing High-sensitivity Troponin Testing
Implementing high-sensitivity cardiac troponin assays into acute-care settings require a multidisciplinary approach. The laboratory plays an important role in driving this effort, as process changes affect key personnel across disciplines. The change may impact hospital leaders, ED clinicians, cardiologists and nurses, and successful adoption of the testing relies on engagement and education about potential new workflows including:
- A change in serial redraw frequency
- A rise in identified myocardial injury
- An increase in cardiology consultations
- Modifications to clinical cutoff points and consideration of sex-specific reference ranges
- A difference in results reporting to whole numbers (ng/L)
Learn more about the advantages of high-sensitivity troponin tests.
Explore the benefits of Access hsTnI, a high-sensitivity cardiac troponin assay.

 English
English





